eosinophilic pneumonia
- related: Pulmonology
- tags: #pulmonology
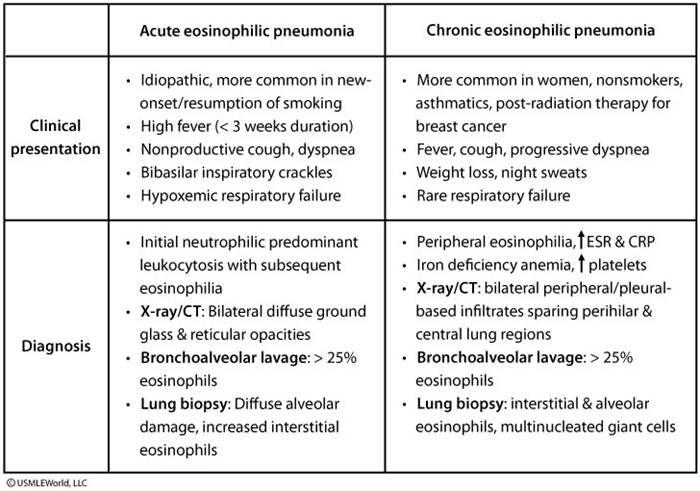
This patient's presentation suggests eosinophilic pneumonia, which can be further divided into acute (AEP) and chronic (CEP) eosinophilic pneumonia. AEP typically follows a rapid course and is more common in smokers. CEP patients are usually nonsmokers, and over 50% have a history of asthma (preceding or after symptom onset).
CEP presents with insidious onset of fever, cough, progressive dyspnea, wheezing, weight loss (often marked), and night sweats. Unlike in AEP patients, hypoxemic respiratory failure is rare. Chest radiograph shows bilateral peripheral or pleural-based opacities ("photographic negative" of pulmonary edema) sparing the perihilar and central lung regions, which is virtually pathognomonic for CEP. Laboratory studies show peripheral eosinophilia > 6%, elevated erythrocyte sedimentation rate and C-reactive protein levels, and thrombocytosis.
Bronchoalveolar lavage with > 25% eosinophils is highly suggestive of CEP. Lung biopsy usually shows interstitial and alveolar eosinophils with multinucleated giant cells and associated bronchiolitis obliterans with organizing pneumonia. AEP and CEP usually respond within 48 hours to glucocorticoids (intravenous for AEP, oral for CEP) with symptom improvement, resolution of x-ray findings, and decreased eosinophilia. Lack of improvement suggests an alternate diagnosis. Relapses occur in up to 50% of CEP but are infrequent in AEP. Treatment is continued for 3 months with gradual tapering over the next 3 months.